CT Ventilation Imaging
CT Ventilation Imaging is software that shows us how well different areas of the lung are performing. This means we can make sure we protect the healthy areas during radiation therapy.
Cancer and lung function.
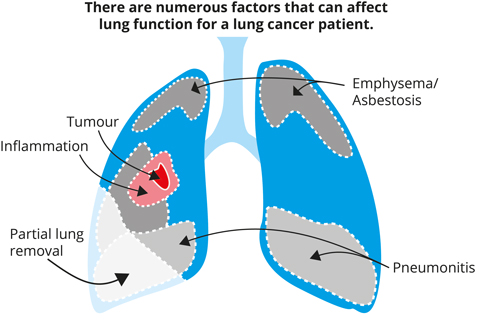
For people with lung cancer, there are numerous factors other than the cancer itself which can seriously impact on the health of their lungs. There can be existing problems such as chronic pulmonary obstructive disorder (CPOD), fibrosis and thickening of the lymphatics in the lung, emphysema, asbestosis and partial lung collapse. As well as this, side effects from cancer treatment can include fluid on the lungs, inflammation and pneumonitis, or even partial lung removal. With so many factors contributing to lung function, it is important to save as much healthy lung tissue as possible during lung cancer treatment, to give patients the best possible chance of survival and quality of life.
Lung cancer is one of the most commonly diagnosed cancers, and one of the most difficult to treat. With 3 out of 4 lung cancer patients being able to benefit from radiation therapy, innovation in this field has the potential to improve the outcomes for tens of thousands of patients in Australia alone. Unfortunately, 30% of patients experience pneumonitis and painful inflammation from the treatment, and for 2% of patients these side effects prove fatal.
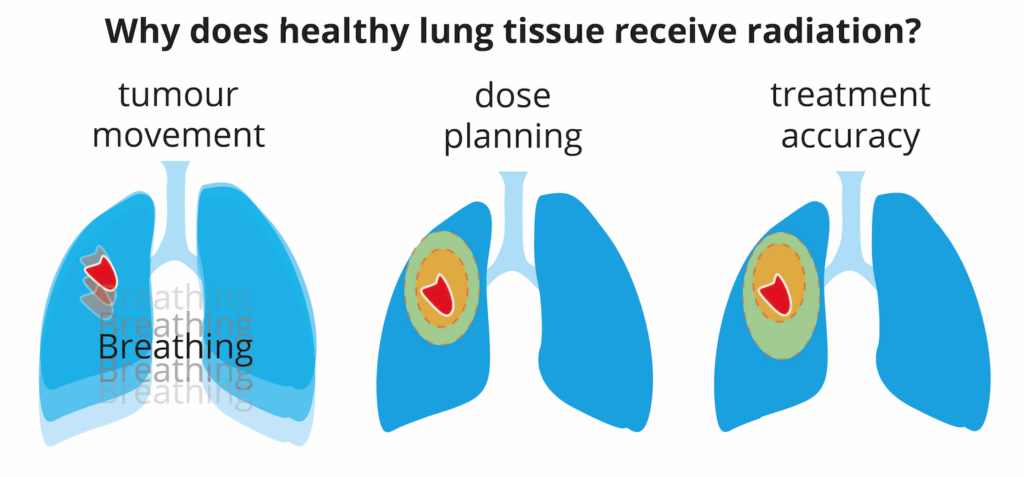
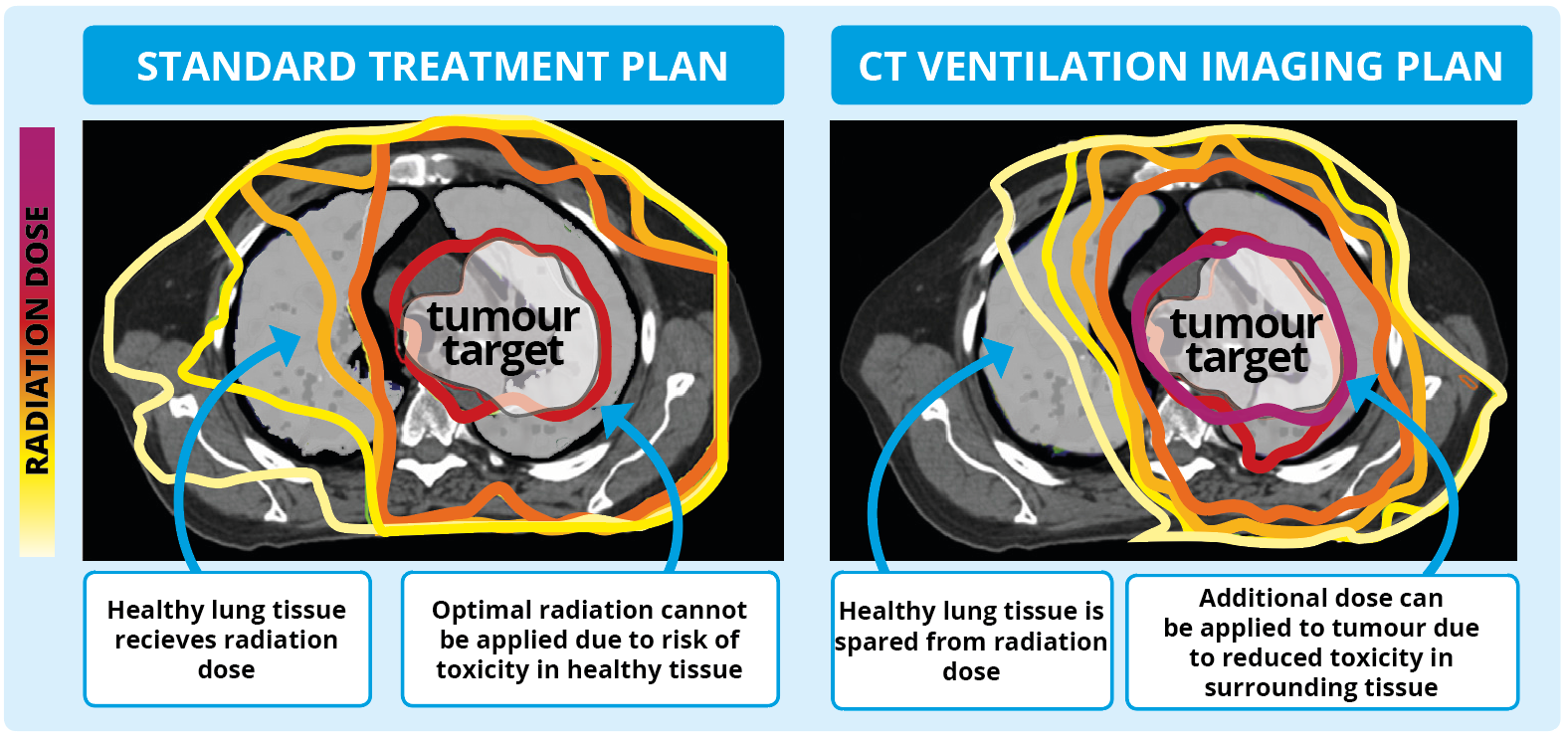
Studies indicate that side effects from radiotherapy could be reduced by avoiding irradiation of healthy (functional) lung tissue. Irradiation of healthy lung tissue happens for a variety of reasons: tumour motion during breathing, the limitations of cancer imaging and treatment accuracy, and treatment planning – designing the strength and location of the radiation beam.
A World-first Solution: CT Ventilation Imaging
Researchers at our institute have developed ‘CT Ventilation’ – a novel software-based solution that can map out the healthy areas of the lung simultaneously while routine pre-treatment scans are carried out. This means that we could improve treatment plans and therefore reduce side effects for cancer patients without conducting any extra scans.
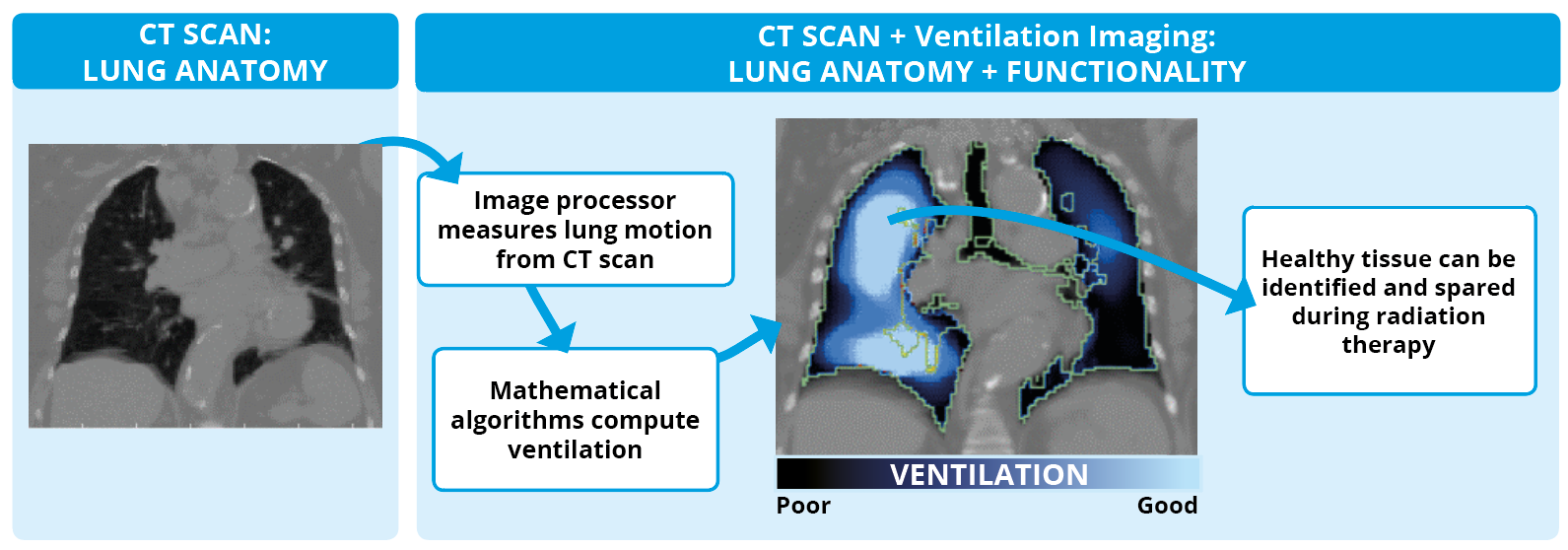
How does CT Ventilation Imaging Work?
- Aquire CT-images of the lung at exhale and inhale states, using breath-hold CT, or 4D-CT (CT imaging which is in 3D and captures the image over time, to show movement).
- Deformable image registration (DIR) software is used to determine a spatial mapping (“deformation map”) between the exhale and inhale CT images.
- Application of a ventilation metric involves quantitative analysis based on the information from the DIR software.
The resulting ventilation image can be superimposed directly onto the anatomic image, providing an added dimension of functional information which is easy to understand and can be of direct benefit in planning a radiotherapy treatment.
Validating CT-ventilation imaging
We have conducted a clinical study at Royal North Shore Hospital testing the physiological accuracy of CT ventilation imaging for use in lung cancer radiotherapy. The physiological accuracy of CT ventilation imaging was assessed via a correlation study against the current gold standard for ventilation imaging, nuclear medicine imaging.
We also quantified the dosimetric impact of CT ventilation imaging for Functional Avoidance Lung Radiotherapy. Functional avoidance is a method of treatment planning which tries to avoid irradiation of high-functioning (well-ventilated) lung regions.
The results of this study were published in the European Journal of Cardio-Thoracic Surgery, with our method attaining similar results to the gold standard for ventilation imaging.
Intellectual property
US Patent – PCT #7668357 Method and system for using computed tomography to test pulmonary function – granted 23 February 2010
Contact
For more information on this project, contact Professor Paul Keall
Paul.Keall@sydney.edu.au