The Australian MRI-Linac Program
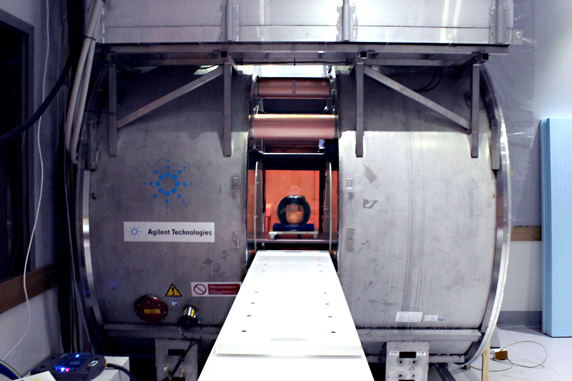
The Australian MRI-linac program is a 16 million dollar project to build a Magnetic Resonance Imaging (MRI) device combined with a Linear Accelerator, which is used to treat cancer using radiotherapy. The goal of the project is to develop next generation cancer therapy equipment, in which changing patient anatomy and physiology can be seen during treatment. This will dramatically improve the accuracy of radiotherapy, directly improving outcomes for cancer patients. The program is driven by the research collaboration of the ACRF Image X Institute, the Ingham Institute for Applied Medical Research in Western Sydney, and the Centre for Medical Diagnostic Technologies at the University of Queensland. The Australian MRI-linac program is led by Professor Paul Keall.
(Video courtesy of the Ingham Institute)
Benefits and challenges
An MRI/linear accelerator has a number of benefits compared to existing image guidance technology.
- Excellent soft tissue contrast
- No imaging dose
- 3D Volumetric data
- No fiducial markers
However, combining an MRI with a Linear accelerator is a momentous engineering challenge. MRI utilises strong magnetic fields to form images; these fields will influence many aspects of normal Linac operation. In turn, the presence of the linear accelerator interferes with the MRI image acquisition process.
Through the Australian MRI-Linac Program, we plan to overcome these challenges and develop a new cancer radiotherapy system that can image tumours as they move within the body, and target the radiation beam to follow this motion. Ultimately, we expect that the MRI-Linac will improve tumour control and cancer survival, whilst reducing the side effects from radiation therapy, leading to an improved quality of life for cancer patients.
Even beyond the realms of cancer treatment, the MRI-Linac could hold high therapeutic potential – we are also investigating the potential use of MRI-guided radiotherapy to treat heart rhythm disorders.
Background
One of the main problems in conventional radiotherapy is that tumours and their surrounding organs move around during and between treatments due to breathing, digestion and other physiological processes. This can result in the tumour receiving less radiation than was intended, or the healthy tissue receiving more. This in turn can decrease the efficacy of radiotherapy, whilst increasing the detrimental side effects.
In order to rectify this effect, image guidance in radiotherapy is becoming increasingly common. Image guidance refers to imaging the patient between or during treatments in order to obtain information about any anatomical changes. There has been a steadily increasing uptake of image guidance techniques in the clinic demonstrating the efficacy of such techniques. However, current techniques suffer from a number of shortcomings, such as:
- Poor soft tissue contrast – this can make it difficult to visualise the tumour from its surroundings
- Secondary imaging dose – Imaging dose can result in non negligible increase in secondary cancer riskIn turn, this limits how often some techniques can be utilised.
- Reliance on fiducial markers – Some techniques require the surgical insertion of a number of small metallic markers
- Assumption of correlation between surface anatomy and internal anatomy – Some techniques use information about movement of the patient surface to infer information about the internal anatomy. This assumes a correlation which may or may not exist.
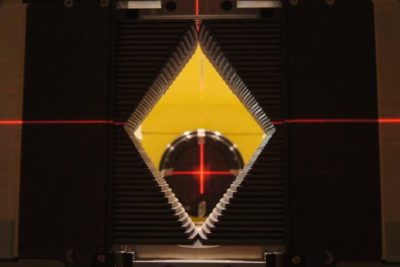
(Image courtesy of the Ingham Institute)
Contact
For more information and enquiries contact Dr David Waddington.