Robotic QA Phantom – 6DoF
The robotic phantom quality assurance device accurately mimics tumour motion, ensuring safe implementation of radiotherapy technologies in the clinic.
In order to measure the accuracy of radiation therapy, quality assurance (QA) processes are conducted using special QA devices. In the clinic, we use these devices to measure whether the radiation therapy system is delivering treatments accurately in terms of the positioning and strength of the radiation dose. In research settings, these QA devices allow us to test whether our new technologies are performing as expected. They act as a ‘ground truth’ for experiments, allowing us to simulate real treatments and make necessary adjustments before moving towards clinical trials with patients.
Radiation therapy is a rapidly improving technology. Advances in real-time imaging and motion adaptation are leading to more accurate, effective treatments and fewer side effects for patients. We can see this tumour motion and track it far more accurately than ever before, even when the tumour moves due to breathing, coughing or digestion.
The Challenge
As radiation therapy technology becomes more accurate, we run in to a problem. Existing QA devices can’t validate our work to the high level of accuracy we’re now achieving. At Image X, we’re measuring the motion of tumours with sub-mm accuracy as they move in every axis direction, and even as they rotate.
To validate our results we needed to develop a device that essentially mimics the behaviour of a tumour inside the body, during treatment. There are QA devices that can validate the radiation dose, and/or tumour motion along 1 or 2 axis, but none that can comprehensively validate all of the motion and accuracy variables required.

Our Solution
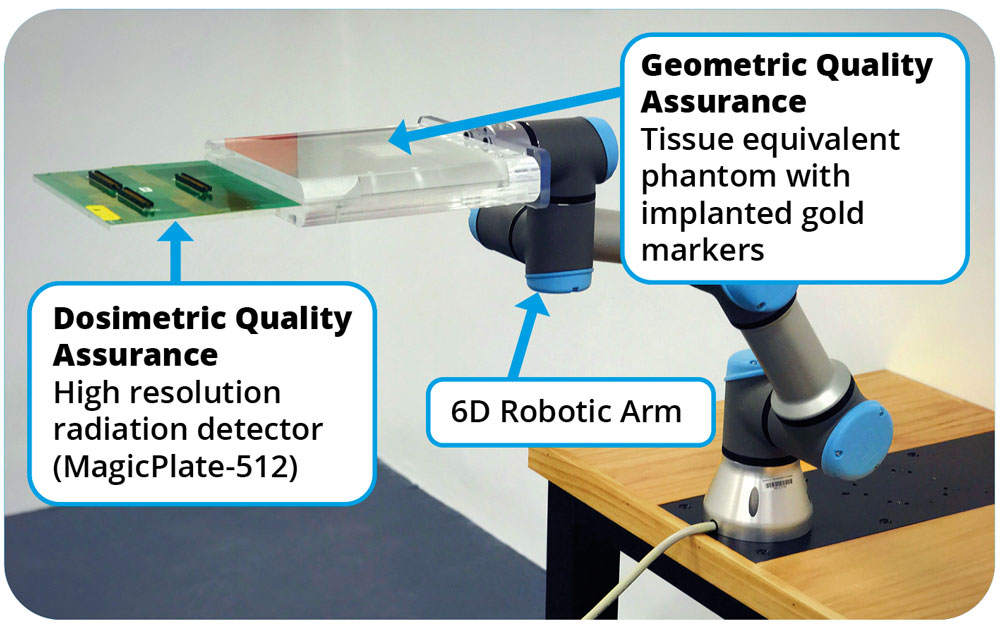
We’ve developed the first robotic phantom quality assurance device that accurately mimics tumour motion in 6 degrees of freedom, ensuring safe implementation of radiotherapy technologies in the clinic.
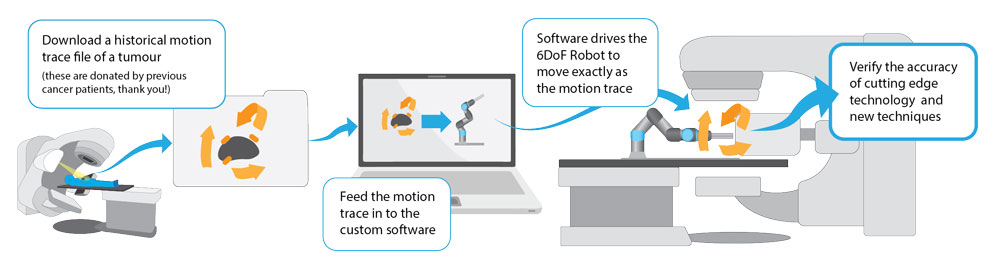
The device is made up of a robotic arm, a custom made plate that has tissue-like properties a plate that measures radiation, and software that controls the movement of the robot. In addition to this, we have a set of ‘tumour motion traces’. These motion traces are readings of real tumour motion, captured during patient treatments.
We feed the motion trace in to the software we’ve developed, which drives motion of the robot.
How it Works
Software Interface
Liver tumour motion trace (Double speed)
Open Source
This project is now available open source via Github, where he have provided the software as well as specifications for equipment needed, and full documentation.
View the project on Github here.
Clinical Trials So Far
TROG 17.03 LARK Trial
For this trial, the device was used to QA the accuracy of our liver motion tracking technology.
The LARK trial looks at treatment outcomes and treatment efficiency when incorporating KIM with SABR treatment to treat people who have primary or secondary liver cancer. The KIM system tracks tumour movement as the patient breathes.
TROG 18.01 NINJA Trial
For this trial, the device was used to QA the accuracy of our prostate tracking technology.
The NINJA Trial is a randomised trial comparing two emerging radiotherapy regimens for prostate cancer, across 3 sites in Australia.
Publications
- S. Alnaghy et al., Phys. Med. Biol. 64 105021 (2019)
- Shi K. et al., Med Phys. 47(12):6068-6076 (2020)
Future Work:
- Create a phantom with a lung insert for quality assurance of markerless tracking systems in lung cancer.
- Concurrent geometric and dosimetric quality assurance with a radiation detector or films.
- QA other real-time tracking systems such as depth sensors as used in the Remove the Mask Project.
Use Cases
Radiotherapy technology: KIM, Potential technologies: Cyberknife, MRI-Linac, ….
Adaptation: Gating, MLC tracking, Couch tracking
Accuracy: < 0.2 mm and <0.6 deg
Cancer sites: liver and prostate
Potential sites: pancreas, lung